A patient calls 911 for chest pain. The discomfort is desribed as a retrosternal pressure. It is worse with coughing and slightly improved with rest. The patient reports a productive cough and subjective fevers. The patient is awake and alert. Past medical history is significant for COPD, asthma, and tobacco abuse.
BP: 180/100
P: 140
R: 16
P: 140
R: 16
Sp02: 92% on room air.
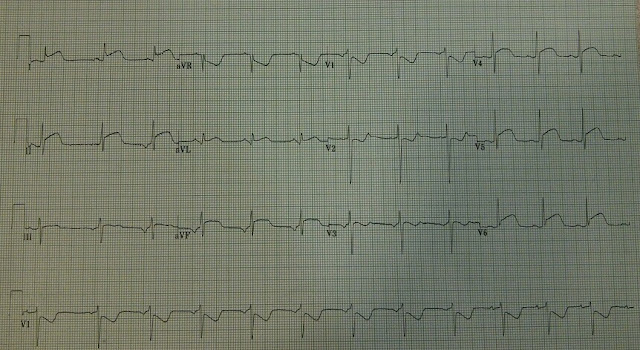
Prehospital 12 lead:
12 lead ECG interpretation:
Sinus tachycardia, left ventricular hypertrophy, diffuse ST segment depression and T wave inversion (inferior, anterior, lateral leads) consistent with strain, possible anterior-lateral ischemia
Left ventricular hypertrophy refers to an increase in heart muscle mass. This change is usually secondary to advanced and uncontrolled hypertension. Simply put, the ventricular muscle increases in order to pump against the increased (hypertension-mediated) afterload. Left ventricular hypertrophy manifests on the ECG as increased R wave amplitude (height). There are several scoring systems for LVH and some have rather poor sensitivity. The definitive diagnosis of LVH is by echocardiogram. The echocardiogram actually measures the thickness of the left ventricle.
General ECG features of LVH:
- Left axis deviation
- Repolarization changes (ST depression)
- Increased QRS amplitude (tall R waves, deep S waves)
Electrocardiographic voltage criteria for LVH:
The STRAIN of hypertension:
Ventricular strain is usually associated with hypertensive heart disease and coronary artery disease. It is a type of ECG pattern seen in ECGs consistent with ventricular hypertrophy. It usually indicates a compensatory response to uncontrolled hypertension and may indicate underlying ischemia. Electrocardiographic criteria for ventricular strain includes:
- ST depression greater than or equal to 1mm in lateral leads I, aVL and V4-V6
- Direction of the T wave usually opposite an upright QRS complex
- Downsloping ST-T segment, rapid upslope
http://www.medscape.com/viewarticle/504439_3
Case Resolution:
The patient was transported to a local emergency department. The tachycardia resolved following administration of intravenous fluids. Repeat ECGs showed some improvement of the ST segment abnormalities. Given the patient's hypertension and ECG changes, blood was also sent to the lab for cardiac enzyme analysis. Cardiac enzymes remained negative throughout the patient's hospital stay. The patient was diagnosed with bronchitis. The patient was admitted to the hospital for symptom management, blood pressure control, and cardiac stress testing.
EMS Pearls:
- Fix the rate first! Tachycardia, by itself, increases myocardial oxygen demand and produces ST segment changes
- Left ventricular hypertrophy causes ST segment changes that resemble ischemic patterns
- The "strain" pattern, characterized by ST sepression and T wave inverison, is associated with underlying coronary artery disease
- LVH is a common response to long standing and uncontrolled hypertension