An elderly male patient is transported to the emergency department following a syncopal episode. The patient reported feeling lightheaded, and experienced two witnessed syncopal episodes lasting for several minutes. Symptoms were made worse when standing up. The patient denied chest pain and reported some mild dyspnea. The patient had been in his usual state of health. The patient's medical history is significant for a tibial fracture several months prior.
Vitals:
Afebrile
BP: 72/P
P: 100
R: 24
Sp02: 92%, poor waveform, on NRB
Physical exam:
Pt is diaphoretic and alert.
Lungs are clear bilaterally.
The patient's abdomen is soft and non tender.
No evidence of lower extremity edema.
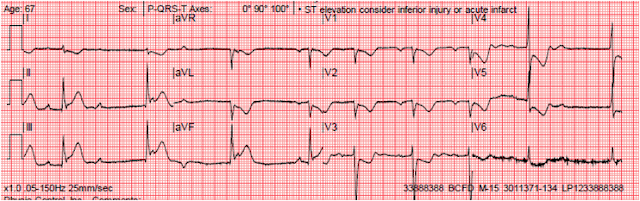
(Prehospital) 12 lead ECG:
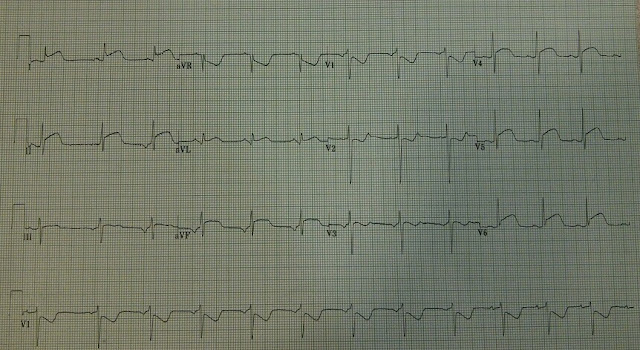
Upon arrival at the hospital, large bore IV access was secured. A FAST (Focused Assessment with Sonography for Trauma) exam revealed no obvious free fluid and no obvious pericardial effusion. The abdominal aorta appeared grossly normal. The patient remained alert and responded to a bolus of IV crystalloid. A repeat ECG was obtained following another pre-syncopal event in the emergency department.
12 Lead ECG Interpretation and Discussion
On the repeat ECG, a sinus rhythm is present. The electrical axis is physiologic. Artifact interferes with the tracing in the inferior limb leads. ST segment elevation is present in aVR, V1, and V2. The ST segments appear horizontal in shape. That particular morphology is concerning for ischemia. While some mild ST segment depression is present in lead I, there are no clear cut reciprocal changes. The evolving changes suggest a septal wall myocardial infarction.
Final Interpretation
Sinus tachycardia, septal ST segment elevation myocardial infarction
(WRONG!)
Case Conclusion
The patient was transported emergently to the cardiac catheterization lab. The patient's coronary arteries were CLEAN and without evidence of disease. An emergent echocardiogram showed a severely dilated right ventricle with concurrent diastolic dysfunction. The clean coronary arteries and echocardiograpghic findings combined point to a massive pulmonary embolism as the cause of the patient's symptoms. Another subtle clue to this diagnosis was the hypoxia that persisted with high flow oxygen administration.
Though not all that elevates is a STEMI, field providers should nevertheless focus on identifying worrisome ST segment changes. The patient's initial ECG was somewhat non-specific. Though close inspection can reveal some slight ST segment elevation of less than 1mm in aVR and V1, it certainly did not meet standardized criteria for STEMI. The second ECG, however, represents a clear-cut evolution. ST segments have become more pronounced (elevated) in the septal leads. The increase in elevation combined with the horizontal plateau of the ST segments in leads V1-V2 suggest an evolving myocardial infarction- or an alternative diagnosis.
The patient presented with a syncopal episode and profound hypotension. Any number of emergent medical conditions can present with those complaints. Pulmonary embolism, internal bleeding, and aortic dissection must be considered in the initial assessment of the hypotensive patient. Unfortunately, there are no "classic" electrocardiographic findings associated with a large PE. That said, the following features can be seen in the setting of a pulmonary embolism.
PULMONARY EMBOLISM ECG FINDINGS
Sinus tachycardia
Right bundle branch block or incomplete right bundle branch block
Deep S wave in lead I, Q wave in lead III, and an interveted T wave in lead III (S1, Q3, T3)
- T wave inversions
Right axis deviation
ST segment deviation (depression and elevation)
Sinus tachycardia and right bundle branch block may suggest "heart strain." These are electrical manifestations caused by the right ventricle that is pumping against a greatly increased pulmonary resistance.